Highlighted Projects
Reducing Hospital Acquired Delirium
Hospital-acquired delirium is serious, leading to increased falls, pressure ulcers, length of stay (LOS), cost, patient institutionalization, and patient and caregiver distress. In addition, it is associated with mortality rates as high as 35-40% within one year in older patients who develop delirium. Because hospital-acquired delirium is often under-recognized and prevention and treatment involves multi-disciplinary care coordination, comprehensivea programs to decrease delirium are often lacking.
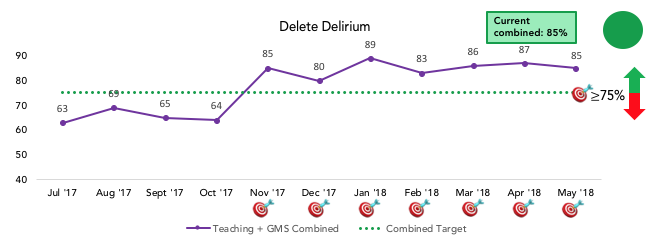
UCSF Health rolled out a Delirium Reduction Campaign in September 2016 and the Medicine units (14M, 14L, 15L) launched delirium screening, prevention, and treatment interventions in January 2017. As of May 2018, nursing compliance with AWOL (delirium risk) screening is > 90%, compliance with Nu-DESC (delirium) screening is > 90%, and physician activated delirium order set compliance is > 85% on the medicine units. LOS in patients with delirium on medicine units has thus far decreased by 1.1 days, or a 10% decrease. However, there are still ongoing quality gaps and ongoing needs for PDSA cycles to continue to improve our processes and maximize the impact of the Delirium Reduction campaign for our patients, families, and staff.
A few examples of areas of ongoing need include:
- Engagement of patients and families (when possible) around delirium education, prevention and treatment strategies
- Ensuring elements of delirium non-pharmacologic protocol are being followed and achieve compliance goals; audit and feedback of compliance to unit RNs, PCAs, staff
- Ongoing education/outreach to Medicine UBLT unit RNs, PCAs, staff re: AWOL/Nu-DESC screening, non-pharmacologic protocol, outreach to providers when patients screen AWOL or Nu-DESC positive
- Pilot of new APeX sidebar notification to providers of a patient’s AWOL or Nu-DESC positive screen and reminder to order Delirium Orderset and evaluate patient for underlying cause(s) of delirium
- Provider interviews to determine if Sidebar Notification is driving anticipated behavior change and to test overall user-interface/usability
Team Members: Stephanie Rogers, Catherine Lau, Adeena Khan, Jenica Cimino, Jennifer Miranda, Rendi Solis, Tatiana Urisman, Carine Davila, Serge Gajic, Lev Malevanchik, Amanda Johnson, Brian Holt
Improving the Patient Experience
Improving the patient experience remains a high priority for our Division and Health System. We have adopted a multi-pronged approach to patient experience improvement, and will briefly highlight a few ongoing initiatives here.
All hospital medicine providers are greatly encouraged to attend the Center for Enhancement of Communication in Healthcare training sessions. In addition, Division members have provided shorter training sessions during our monthly QI lunch. Objectives of the Enhancing Relationship Centered Skills course include:
- Understand the importance and value of effective communication
- Build rapport and relationships with others
- Acknowledge communication barriers, with special attention on the computer and time limitations
- Recognize another’s perspective and concerns
- Negotiate an agenda for an encounter
- Ask questions using skilled open-ended inquiry
- Listen reflectively and respond with empathy
- Collaborate on a plan that others can follow
We also partner closely with UCSF Post-Baccalaureate students to train them in communication best practices, shadow teams during bedside rounds, and provide real-time feedback to clinical teams on their performance with suggestions and comments from the patients they are caring for.
We have an operational Hospital Medicine Patient and Family Advisory Council and actively recruiting additional members under the leadership of Erin Yao-Cohen, James Harrison, and Michelle Cai The Hospital Medicine PFAC will serve as a rich and invaluable resource for us as we continue to design and implement new PDSA cycles to improve the patient and family experience.
Team Members: Erin Yao-Cohen, James Harrison, Jenica Cimino, Michelle Cai, Catherine Lau
Reducing Readmissions
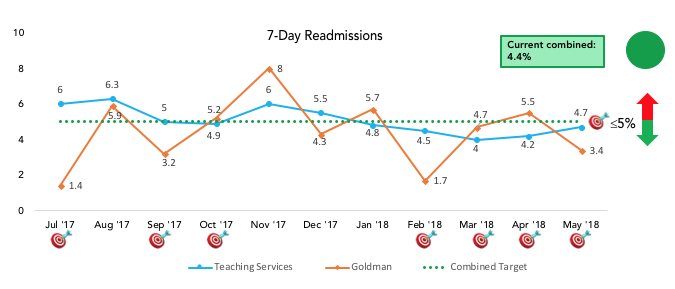
Improving transitions of care from the inpatient to the outpatient setting and reducing readmissions has been a long-standing focus of our QI program. More recently, we have pivoted from focusing on reduction of 30-day readmissions to reducing 7-day readmissions based on several recent publications concluding that early readmissions are more directly in the control of hospital-based providers than later readmissions.
Our first year in drilling down to 7-day readmissions has been spent understanding the current state, determining our targets, performing a thorough gap analysis, and creating a driver diagram that also helped to illuminate our countermeasures.
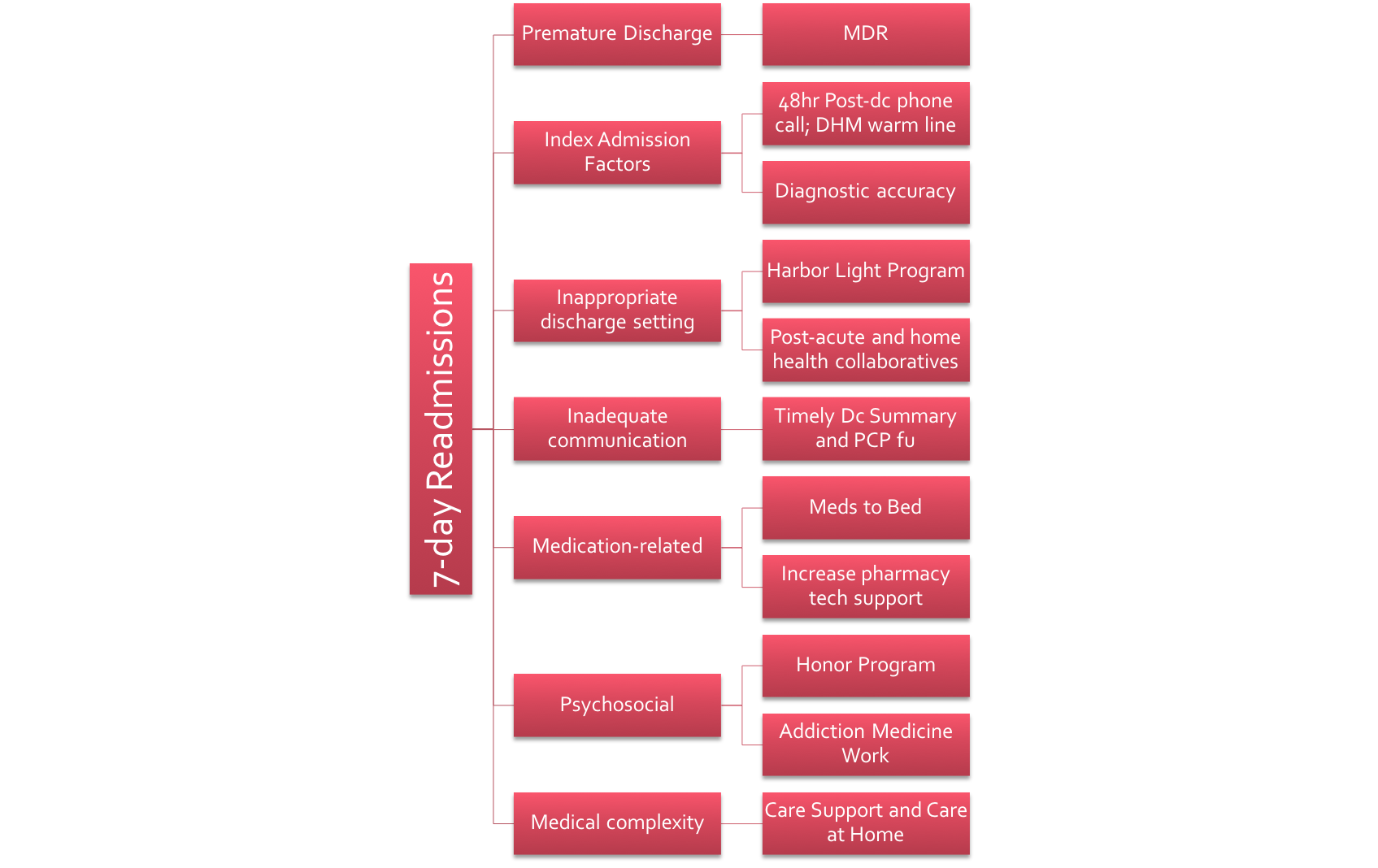
Thus far, we have been successful in continuing our close partnership with the Health System Excellence in Transitions of Care Committee, are actively participating in Office of Population Health and Accountable Care strategic initiatives particularly around the Medicare Shared Savings Program (MSSP), and continue to work closely with our case management, social work, administrative staff, and residency program to ensure optimal transitions of care. These efforts have resulted in a decrease of our 7-day readmission rate from 5.6% to < 5% over the past year.
Team Members: Katie Raffel, Michelle Mourad, Catherine Lau
Reducing Treatment of Asymptomatic Inpatient Hypertension
Asymptomatic elevated blood pressure in the hospitalized patient is common (50-70%), is over-treated with IV medications despite lack of evidence supporting clear benefit, may cause harm due to resultant hypotension, contributes to unnecessary added costs to a hospitalization, and results in high cross-cover burden to providers.
The #NoIVforHighBP value improvement campaign spent the past year:
- Delivering an educational campaign to medicine attendings, residents, students, nurses, and unit directors on tips for the optimal management of asymptomatic inpatient hypertension
- Modified standard vital sign notification parameters in the core admission order set from BP > 160/90 to BP > 180/90
- Performing audit and feedback of data to all clinical teams
- Successfully reduced utilization of IV anti-hypertensives to treat asymptomatic hypertension by over 25%
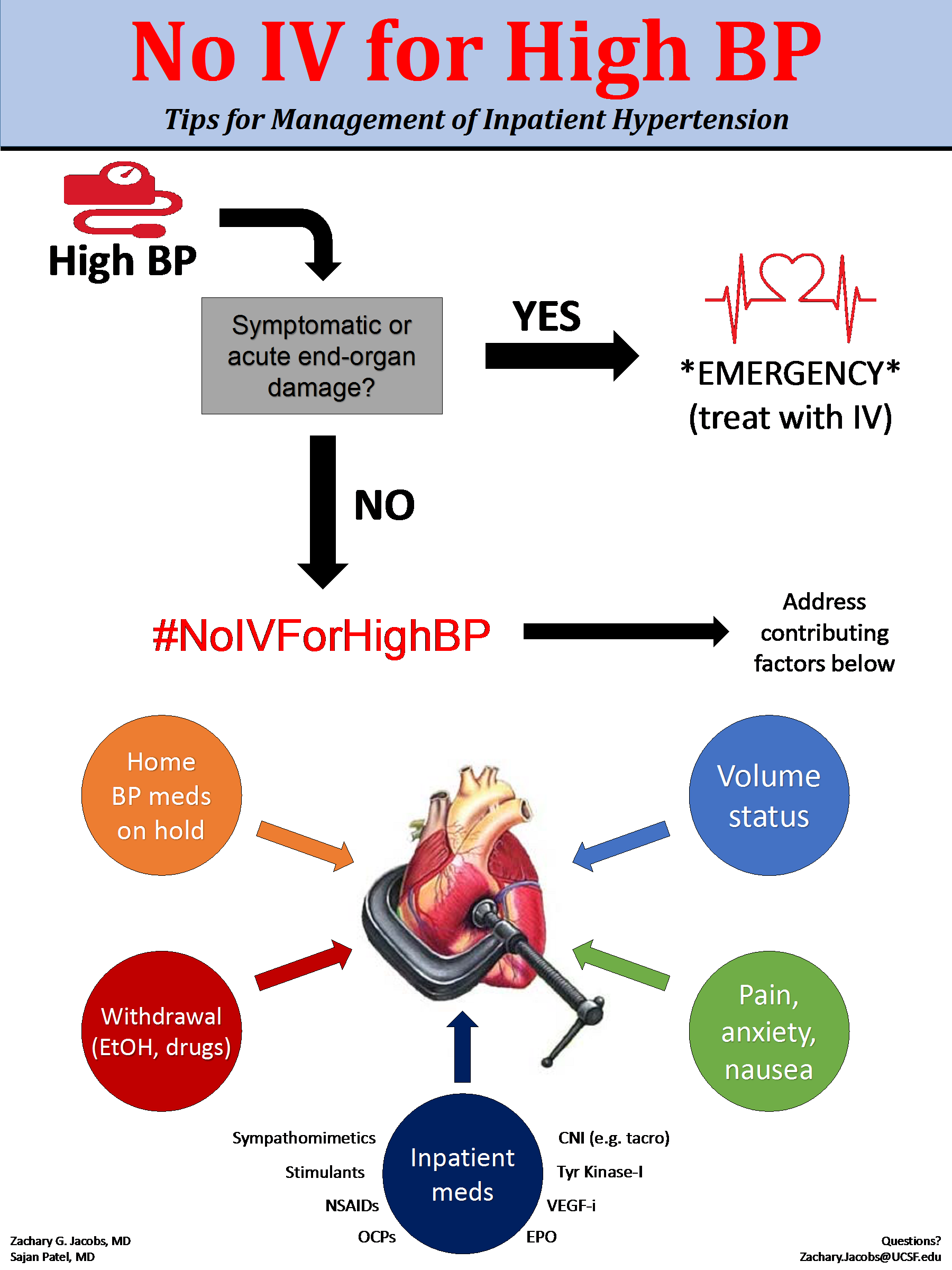
Team Members: Saj Patel, Zac Jacobs
Promoting Sleep Project
If you or your loved one has spent a night in a hospital, you know firsthand how challenging it can be to get a good night's sleep. Whether it is fluorescent lighting, the noise or the constant interruptions due to medication administration, vitals, or blood draws, we often hear about these common disruptors of sleep from our patients. While few studies specifically link sleep and patient outcomes, most physicians agree that the connection is obvious: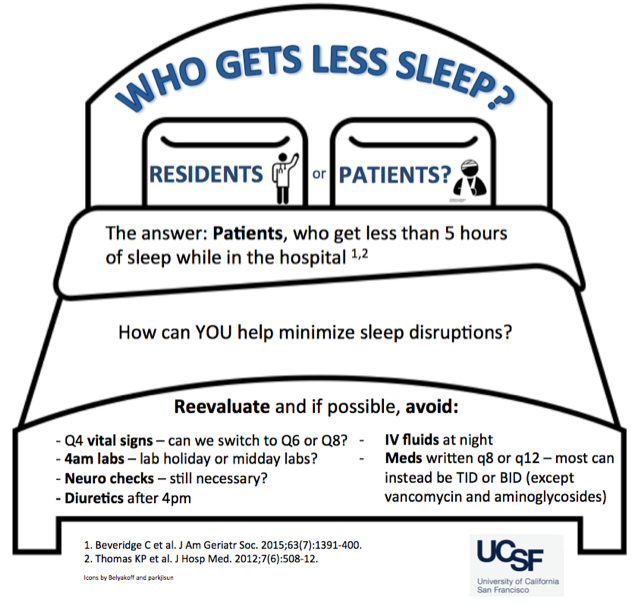
"Patients need sleep. If they get more of it, they'll likely recover faster."
In addition, the "quietness of the hospital environment" is a patient experience question in the nationally administered HCAHPS survey, so health systems have a keen interest in tackling this important issue.
The good news is there are several low-hanging fruit solutions that we are implementing at our institution to promote sleep and an optimal healing environment for our patients. Interventions include:
- Modified the admission order set and daily orders to allow reduced nighttime vital sign checks.
- Developed a bedtime checklist for nurses and patient care assistants to assess patients for sleep readiness in the hospital, including turning off the TV and lights and providing ear plugs if necessary.
- Developed a machine learning algorithm that will be embedded in the EHR to accurate predict which patients are eligible candidates for sleep promoting vitals based on clinical stability, and building prompts within the EHR to notify providers to order sleep promoting vitals.
- Validating a “sleep opportunity” metric that determines the greatest length of time between nighttime orders, medications, and vital sign checks, and determining if this metric correlates with actual patient sleep.
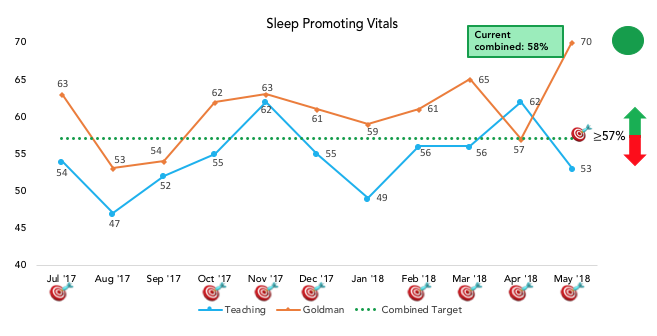
Team Members: Saj Patel, Ari Hoffman, Nader Najafi, Kristen Kipps, Timothy Judson
Improving Communication with Patients with Limited English Proficiency
Patients with limited English proficiency (LEP) face multiple barriers in their health care, leading to significant disparities and worse outcomes. Providing professional interpreter access to patients with LEP can mitigate some of these barriers, but this endeavor is not easy. One of the reasons is a lack of understanding of whether interpreters are being used. Previous efforts to measure professional interpreter use were done via surveys of providers or via interpreter use across systems, which are too unreliable or broad to engage in focused quality improvement projects.
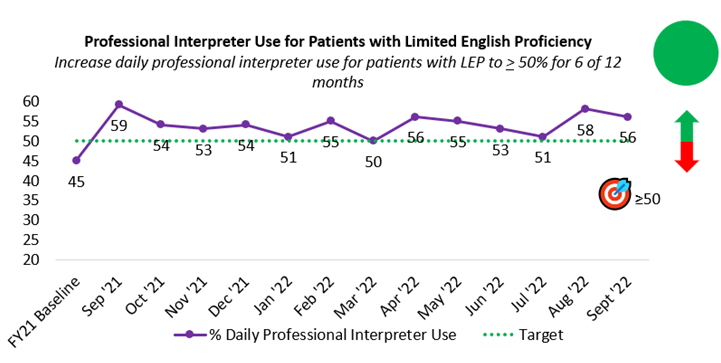
Our group in the Division of Hospital Medicine (DHM) launched a project in 2018 to use data to understand whether our hospitalist physicians were using professional interpreters daily with their patients with LEP. Our QI metric started by measure video interpretation and grew over five years to measure video, phone, and in person interpretation. Our baseline was 27%, and this grew to 55% by the time our project ended. This metric was a true north metric for four years in a row, and we outpaced our target each year!
As a result:
- more patients with LEP got daily interpreter access with their doctors
- the health system purchased more interpreter iPads to use with our patients
- we performed audit and feedback with medical teams to analyze situations when interpreters could have been used
- we educated members of DHM and other divisions about the use of interpreters